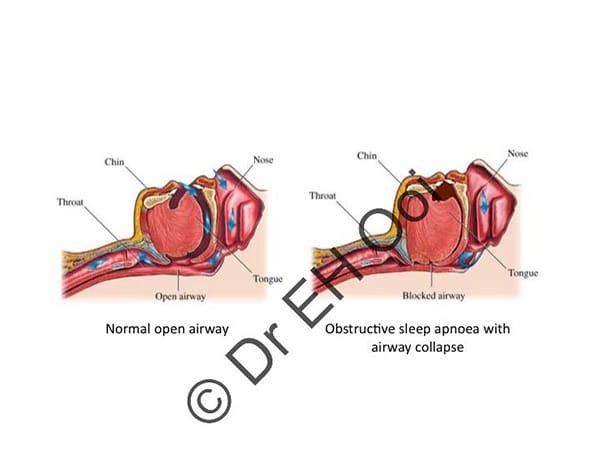
Snoring is due to obstruction at either one or multiple levels of your nose and throat. You may have “simple snoring” where your oxygen levels are normal or “obstructive sleep apnoea” (OSA) where you stop breathing briefly with a decrease in your oxygen levels. OSA can lead to daytime sleepiness, waking up unrefreshed, and cardiovascular events (e.g. heart attacks, high blood pressure, and strokes).
How do I know if I have OSA?
You need to have a sleep study done, which is where specialised monitoring is used to diagnose your breathing, heart rate, oxygen levels etc as you sleep overnight in a sleep lab. This is done through a referral to the respiratory sleep physicians and/or to private sleep labs. In most cases, a limited modified sleep study can be done in your own home. Patients can be referred by their GP or ENT for a sleep study. The medicare rebate for a sleep study is for patients with a high probability of obstructive sleep apnoea based on a STOP‑Bang score of 3 or more, an OSA50 score of 5 or more or a high risk score on the Berlin Questionnaire, and an Epworth Sleepiness Scale score of 8 or more OR the qualified adult sleep medicine practitioner or consultant respiratory physician determines that assessment is necessary to confirm the diagnosis of a sleep disorder. Adelaide ENT surgeons require patients to complete this questionnaire to assess the probability of the patient having sleep apnoea in order for us to refer you for a sleep study.
How do I treat snoring?
Weight loss, changes in sleeping position, oral dental appliances, surgery as below or CPAP (for OSA) are usually sufficient to manage your snoring.
Nasal – septoplasty and turbinate reduction
Throat – UPPP (uvulopalatopharyngoplasty) and/or radiofrequency tongue reduction.
Professor Eng Ooi has been treating patients with OSA using this surgical technique for selected patients with snoring and obstructive sleep apnoea. Successful surgery means you may not need to use CPAP or snore loudly. Professor Ooi was part of the Multi-Centre NHMRC trial performing this surgical technique to assess its overall effectiveness in patients with moderate to severe OSA. The trial was published in JAMA, a high impact factor journal (IF 45.5), demonstrating that patients who had the surgery had a significant reduction in severity of their OSA, less daytime sleepiness, improved sleep quality and reduction in partner reported snoring. Please refer to the published article for a detailed explanation of the results.
Please ask for a referral to see Professor Ooi if you are interested in surgery for your obstructive sleep apnoea.
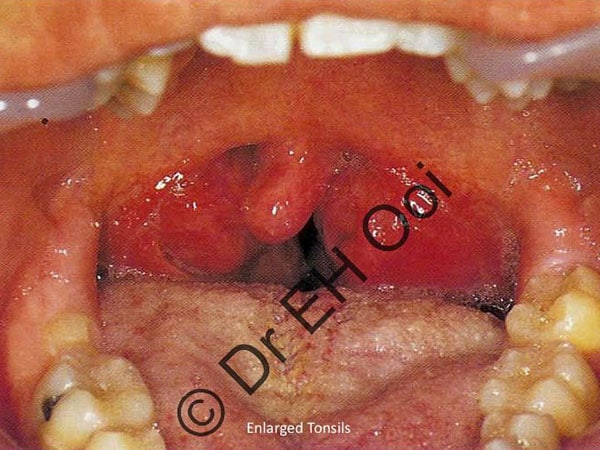
What is a UPPP?
It is a procedure under general anaesthesia to remove your tonsils, part of the uvula and the redundant tissue of the soft palate. Professor Eng Ooi uses a specialised technique to conserve and stitch your soft palate to produce a more natural appearance. The traditional technique of cutting the uvula off and squaring off your soft palate is believed to cause more globus (sensation of a lump) and swallowing difficulties. Professor Ooi uses newer techniques to minimise these problems.
What is radiofrequency tongue reduction?
It is a procedure using coblation (a controlled non-heat driven process using radiofrequency energy and plasma to gently remove tissue) and a specialised wand to “shrink” the bulky tongue, therefore creating more space for you to breathe at night. There are risks with the procedure and A/Professor Eng Ooi will discuss these with you so that you can make an informed decision about your surgery.
What is Drug Induced Sleep Endoscopy (DISE)?
It is an assessment of your upper airway and areas of collapse or narrowing to mimic what you are doing when you are “sleeping” under a general anaesthetic. It is used in patients who have obstructive sleep apnoea or primary snoring. It allows your ENT surgeon to gain further information of your velum, pharynx, tongue base and epiglottis during a state that mimics “sleep”. This helps the ENT surgeon to decide if multi-level upper airway surgery is suitable for you. This is usually done as a day case procedure and your ENT surgeon will review you back in their clinic to discuss the DISE findings.
New treatments being researched and trialled for obstructive sleep apnoea
Professor Eng Ooi and Dr Himani Joshi are collaborating with Flinders University Sleep Researchers new treatments for obstructive sleep apnoea. These include the use of Reboxetine post-operatively to reduce the risk of oxygen desaturations and airway obstruction during sleep. Another exciting clinical trial our surgeons are involved is using novel minimally invasive nerve stimulators to open up your airway.